Introduction:
Imagine waking up one day and discovering that the numbers that once danced effortlessly in your mind have transformed into an indecipherable jumble, a chaotic mess of lines and shapes. This is the reality for RFS, a man whose extraordinary journey reveals the hidden complexities of the human brain. Stricken by a rare degenerative condition known as corticobasal syndrome, RFS experiences a world where numbers become an enigma, slipping through his fingers like grains of sand. While he can still recognize letters and symbols, the very essence of numerical understanding eludes him, raising profound questions about perception, cognition, and the intricate workings of our minds. Join us as we delve into the mind-blowing story of RFS, a tale that not only challenges our understanding of numbers but also invites us to explore the remarkable capabilities and limitations of the human brain.
The story of a man who cannot see numbers, referred to by his initials RFS, provides fascinating insights into brain function and perception. RFS suffers from a rare degenerative brain condition known as corticobasal syndrome, which has led to significant cognitive and motor impairments.
Unique Visual Perception
RFS experiences a peculiar phenomenon where, when he looks at numbers, they appear as a jumbled mess of lines, which he describes as “spaghetti.” He can recognize that he is looking at a number but cannot identify which one it is. Interestingly, he has no difficulty seeing letters or other symbols, suggesting that numbers are processed differently in his brain. For instance, he can easily identify the numbers “0” and “1,” which may resemble letters like “O” or “l” and might be processed in a unique way compared to other digits.
Brain Function and Awareness
Research into RFS’s condition reveals that while he cannot consciously “see” numbers, his brain still processes them. Experiments showed that when numbers were embedded with other visual stimuli, such as faces or words, RFS’s brain responded as if he recognized those stimuli, even though he reported not seeing them. This indicates a complex level of cognitive processing occurring despite his inability to perceive numbers accurately.
Implications for Cognitive Science
RFS’s case sheds light on the complexities of visual awareness and cognitive processing. It raises questions about how the brain categorizes and interprets different types of visual information, particularly in individuals with neurological disorders. This unique condition is the first documented case of its kind, providing valuable insights into the nature of perception and awareness in the human brain.
What were the initial symptoms of corticobasal syndrome in RFS?
The initial symptoms of corticobasal syndrome (CBS) in RFS included a range of motor and cognitive difficulties. He began experiencing slowed movements, stiffness, and tremors, which are common early signs of CBS. Additionally, he faced challenges with fine motor skills, making it difficult to carry out learned tasks, such as writing or buttoning a shirt. As the condition progressed, RFS developed more specific symptoms, including a profound inability to recognize, name, copy, or comprehend the digits two through nine. He described these numbers as appearing like a chaotic tangle of lines, which he referred to as “spaghetti.” Despite these visual disruptions, his understanding of mathematical concepts remained intact, indicating that the cognitive processing of numbers was affected differently than his ability to perceive them visually.
Scientific Explanation and Cure
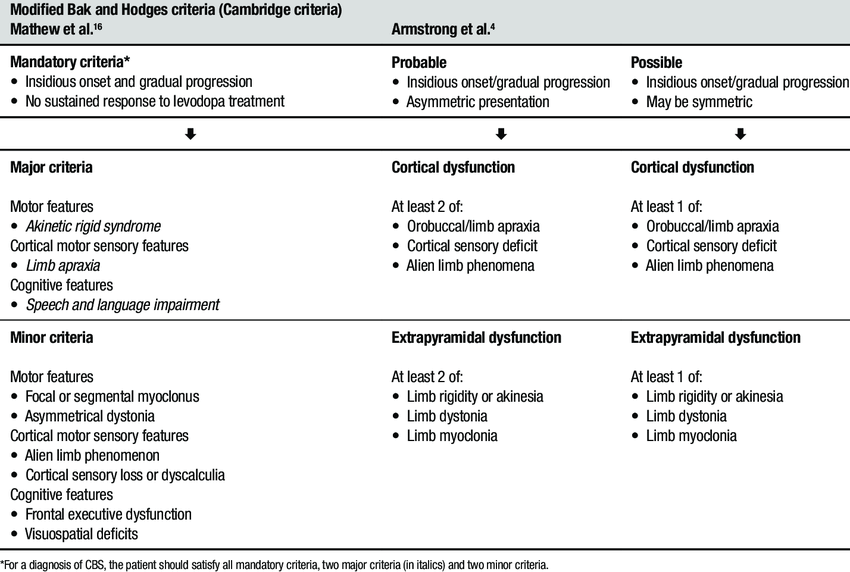
Corticobasal syndrome (CBS) is a rare neurodegenerative disorder characterized by the progressive degeneration of specific brain regions, particularly affecting movement and cognitive functions. The underlying cause of CBS is often linked to the accumulation of a protein called tau in the brain, which disrupts normal neuronal function and leads to cell death. This condition is classified as a form of atypical parkinsonism, sharing symptoms with Parkinson’s disease but differing in its progression and underlying pathology.
Scientific Explanation
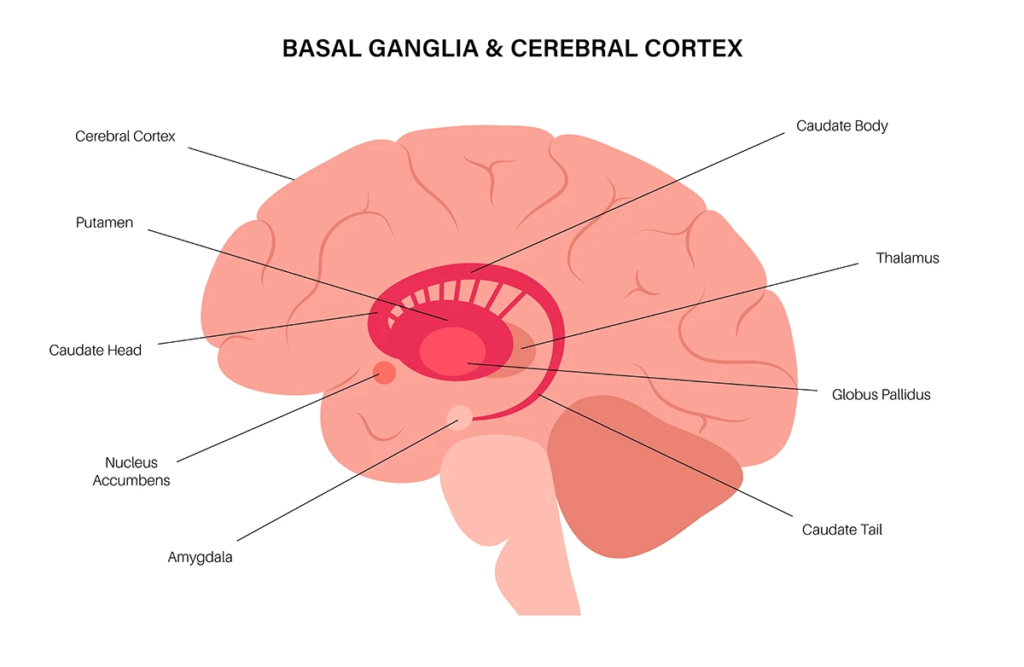
In CBS, the buildup of tau protein leads to the degeneration of neurons in the cortex and basal ganglia, areas of the brain responsible for movement, coordination, and cognitive processing. The initial symptoms typically include:
- Motor Symptoms: These may manifest as stiffness, tremors, bradykinesia (slowness of movement), and difficulty with coordination and balance. Patients may also experience apraxia, which is the inability to perform purposeful movements, and “alien hand syndrome,” where one hand seems to act independently.
- Cognitive Symptoms: As the disease progresses, individuals may face difficulties with speech, memory, and comprehension. Language problems can include difficulty finding words and forming sentences.
The progression of CBS can vary significantly among individuals, but it typically leads to severe impairment in both motor and cognitive functions over a period of six to eight years.
Treatment and Cure
Currently, there is no cure for corticobasal syndrome. Treatment focuses on managing symptoms and improving quality of life. Some approaches include:
- Medications: While there are no specific drugs for CBS, certain medications used for Parkinson’s disease, such as levodopa, may help alleviate some motor symptoms. Cholinesterase inhibitors, like donepezil, can be prescribed to address cognitive symptoms similar to those seen in Alzheimer’s disease.
- Therapies: Physical therapy can assist in maintaining mobility and improving coordination, while speech therapy can help with communication difficulties. Occupational therapy may also be beneficial in adapting daily activities to the patient’s capabilities.
- Lifestyle Adjustments: Maintaining a balanced diet, engaging in regular physical activity, and ensuring adequate sleep can support overall health and potentially slow disease progression.
How does corticobasal degeneration differ from Alzheimer’s disease?
Corticobasal degeneration (CBD) and Alzheimer’s disease (AD) are two distinct neurodegenerative disorders that can both present with a corticobasal syndrome (CBS), characterized by asymmetric movement disorders, apraxia, and cognitive impairment. However, there are key differences in their underlying pathology and patterns of brain atrophy:
Pathology
- CBD is primarily characterized by the accumulation of abnormal tau protein in the brain, leading to neurodegeneration.
- AD, on the other hand, is defined by the buildup of amyloid-beta plaques and tau tangles, which disrupt normal neuronal function.
Brain Atrophy Patterns
- CBS-AD patients show more widespread brain atrophy, particularly in the posterior frontal, temporal, and parietal lobes, compared to CBS-CBD patients.
- CBS-CBD patients exhibit more focal atrophy predominantly in the posterior frontal lobes.
- Both CBS-AD and CBS-CBD show basal ganglia volume loss and relative sparing of the hippocampi.
Clinical Presentation
- CBS-AD patients tend to be younger at symptom onset compared to CBS-CBD patients.
- CBS-AD patients often present with more prominent language and memory deficits, while CBS-CBD patients typically have more pronounced movement disorders.
Are there any genetic factors that contribute to corticobasal degeneration?
Genetic factors play a significant role in the development of corticobasal degeneration (CBD), which is often associated with corticobasal syndrome (CBS). Research indicates that several genetic mutations are linked to the disease, particularly those related to frontotemporal lobar degeneration (FTLD). Here are the key genetic contributors:
Major Genetic Factors
- MAPT (Microtubule-Associated Protein Tau):
- Variants in the MAPT gene, particularly the H1 haplotype, are associated with an increased risk of developing CBD and other tauopathies. This gene is crucial for the stability of microtubules in neurons, and its dysfunction can lead to tau protein aggregation, a hallmark of CBD.
- GRN (Progranulin):
- Mutations in the GRN gene are another significant genetic risk factor for CBD. Progranulin is involved in neuronal survival and inflammation regulation. Deficiencies in this protein can lead to neurodegeneration and are commonly found in familial cases of FTLD, including those presenting with CBS.
- C9ORF72:
- This gene is linked to both familial and sporadic cases of FTLD and amyotrophic lateral sclerosis (ALS). Expansions in the C9ORF72 gene are associated with a range of neurodegenerative diseases, including CBD.
- Other Genetic Factors:
- Additional mutations in genes such as TARDBP, FUS, and LRRK2 have also been implicated in CBS. These genes are associated with various neurodegenerative processes and may contribute to the development of CBS in some individuals.
Genetic Testing and Implications
Despite the identification of these genetic factors, many cases of CBS remain genetically unsolved. Genetic testing can help determine the presence of known mutations and guide diagnosis and management. Understanding the genetic background of CBD can also provide insights into the disease’s pathology and potential therapeutic targets.
Read Related Post
A Global Tour of Bizarre Delights